Neurodevelopment: Unlocking the brain
 Andy Potts
Andy Potts
Much of our neural circuitry is fixed during childhood. Researchers are finding ways to unglue it, raising hopes for treating many brain disorders.
Jon Bardin
Growing up in the suburbs of New York City, Takao Hensch learned German from his father, Japanese from his mother and English from the community around him. “I was always wondering,” he says, “what is it that makes it so easy to learn languages when you're young, and so hard once you begin to get older?”
Today, as a neuroscientist at Boston Children's Hospital in Massachusetts, Hensch is at the forefront of efforts to answer that question in full molecular detail. Language acquisition is just one of many processes that go through a 'sensitive' or 'critical' period — an interval during development when the neural circuits responsible for that process can be sculpted, and radically changed, by experience (see 'Open and shut'). During critical periods, children can make rapid progress at discerning facial features that look like their own, recognizing spoken language and locating objects in space. But within a few months or years, each window of opportunity slams shut, and learning anything new in that realm becomes difficult, if not impossible.
Or maybe not. What Hensch and others in the small, but rapidly advancing, field of critical-period research are finding is that those windows can be prised back open. “For the first time, we are beginning to understand the biology that underlies critical periods,” says Hensch. And that understanding is suggesting ways to intervene in various neural disorders, including intractable conditions such as adult amblyopia, in which information from one eye is not correctly processed by the brain, and possibly even autism. The work could even lead to 'plasticity pills' that enhance learning or help to wipe out traumatic memories.
“What's so interesting about Takao's work is that he has shown that even if you miss these critical periods, you still may be able to go back in and fix things,” says Charles Nelson, a neuroscientist at Boston Children's Hospital, who studies the developmental effects of early social deprivation on orphans in Romania. “The idea that you could intervene later and make up for lost time is compelling.”
The first scientist to popularize the notion of a developmental critical period was the Austrian biologist Konrad Lorenz, whose pioneering work in animal behaviour earned him a share of the 1973 Nobel prize. In the 1930s, Lorenz showed that if he took on the role of a mother goose within a few hours after goslings hatched, the baby geese would follow him as though he were their mother until adulthood. He called this process 'imprinting'.
Dogma, inhibited
The first scientists to explore the neural basis of a critical period were David Hubel and Torsten Wiesel, neurophysiologists at Harvard Medical School in Boston who carried out work on the visual system in the early 1960s. First they discovered that in the adult brain, many cells in the visual cortex respond to signals from only one eye. Then they showed that in kittens that had had one eye sutured shut, individual cells that normally would have fired in response to the closed eye instead responded to the open eye, eventually causing amblyopia1. Shutting the eye of an adult cat did nothing, indicating that cells in the visual cortex were programmed during a key developmental window in the first few months of life.
Hubel and Wiesel lacked the tools to analyse how this programming worked at the molecular level, but they earned a Nobel prize in 1981 for their discovery. Their findings also inspired Hensch, during the 1980s, to change his undergraduate major from computer science and artificial intelligence to neurobiology. “Hubel and Wiesel's work made me realize that there was just so much we didn't know about the actual biology of the brain,” he says.
Hensch got a chance to learn more when he began his PhD work in Michael Stryker's neuroscience laboratory at the University of California, San Francisco (UCSF). Stryker's group, like most researchers in the field, studied the critical period of the visual system as a model of critical periods in general, and had published a series of papers hinting at a new approach to understanding it.
For years, researchers had assumed that the brain's 'plasticity', or its ability to learn during critical periods, was the work of excitatory neurons, which encourage neighbouring neurons to fire. But Stryker's work suggested some kind of involvement by inhibitory interneurons, brain cells that dampen activity in their neighbours. Stryker's team had found that, in kittens, a drug that increases inhibition during the critical period made the visual cortex resistant to Hubel and Wiesel's trick: many neurons in that region began to fire in response to the closed eye rather than the open one2.
Hensch followed up on this work in a collaboration with Michela Fagiolini and her colleagues at the RIKEN Brain Science Institute in Wako, Japan. The researchers looked at the critical period in genetically engineered mice that had slightly reduced levels of γ-aminobutyric acid (GABA), an inhibitory neurotransmitter.
The effect of that reduction was far greater than either Hensch or Stryker had imagined: whereas control mice went through a typical critical period and developed amblyopia when one eye was blocked, mice with GABA deficiencies did not develop amblyopia, or have a critical period at all. Hensch and his colleagues were able to restore plasticity by administering a benzodiazepine, a drug that enhances the inhibitory effect of GABA (ref. 3).
Inhibition, the authors concluded, was a hidden force driving the onset of the visual critical period. “At the time, these ideas were just so counter-intuitive,” Hensch says. “We were turning dogma on its ear.”
Clever mechanisms
Researchers have since begun to clarify the workings of this force. In 2008, Hensch and Alain Prochiantz, a neuroscientist at the Collège de France in Paris, found that when mice first open their eyes after birth, a protein called OTX2 is transported through the optic nerve from the retina to the visual cortex — a marathon in cellular distance.
In the visual cortex, the accumulation of OTX2 sparks a series of events that causes PV interneurons, inhibitory cells that contain parvalbumin (PV), to mature and trigger the beginning of the visual critical period. But this transport takes place only after visual input is received; in mice raised in the dark, no OTX2 arrives in the cortex and no critical period ensues4. “I think this is a pretty clever mechanism from nature,” says Hensch, “because you don't want to be plastic until you know that the periphery is functional and signals are coming in.”
But it was unclear how the PV interneurons triggered the critical period. An important clue came from a group led by Stryker with Arturo Alvarez-Buylla and Sunil Gandhi, also at UCSF. The researchers transplanted embryonic cells that were destined to become interneurons into the brains of young mice, says Alvarez-Buylla, after which the mice “started having two critical periods”. There was the typical critical period, caused by the mouse's own interneurons, and then a later one, triggered when the transplanted interneurons began to mature5.
The transplanted cells, says Stryker, were pushing the system's 'reset' button. In the cerebral cortex of the adult brain, information travels through neural circuits along well-defined paths carved out by mature interneurons, which strongly inhibit some cells and not others. But in the transplant experiment, the maturing interneurons were making numerous weak connections with the older cells and inhibiting all the cells equally, overriding the brain's previously defined circuits.
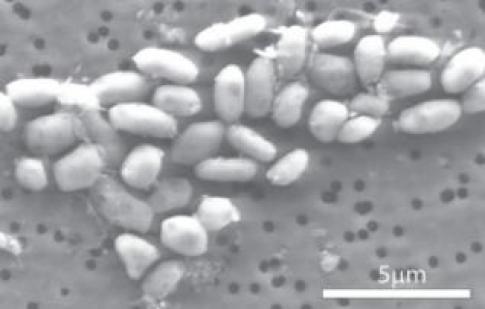
Only as those new cells matured were their connections pruned and strengthened, eventually carving out new permanent circuits. The findings suggested that the same mechanism — PV synapse proliferation followed by pruning — underlies all critical periods.
Hensch and others have found that critical periods do not just taper off as PV interneurons mature. Instead, they are shut down as the brain slams on 'plasticity brakes' — presumably as a way to protect the newly optimized brain circuits from disruption by further input.
Hensch separates these 'brakes' into two categories — structural and functional. The first comprises physical structures such as the perineuronal net (PNN), a complex of macromolecules that attach to PV interneurons around the time that a critical period ends, and that seem to restrict the extent to which a neural circuit can change. Chemical breakdown of the PNNs in adult rats makes their brains prone to being rewired6.
Functional brakes are chemical compounds such as Lynx1 — a molecule, identified by Hensch and his colleagues, that shifts the balance of excitation and inhibition in the cortex by dampening the effect of the neurotransmitter acetylcholine. Experiments in mice show that the amount of Lynx1 in the brain increases at the end of the critical period, and its removal from adult brains, like degradation of the PNNs, seems to restore neural plasticity7.
Hensch says that what he finds particularly compelling about functional brakes is that they are relatively easy to release. One example of this is a behavioural intervention developed by Roger Li and Dennis Levi, optometrists at the University of California, Berkeley, for adults with amblyopia.
People develop amblyopia when problems such as cataracts or crossed eyes disrupt input to one of their eyes during early childhood, often leaving them without three-dimensional (3D) vision. The condition is considered untreatable once the critical period has ended. But when Li and Levi got people with amblyopia to play 40–80 hours of video games with their good eyes patched, most of them reported substantial improvements in visual function8. Describing one subject who was born with crossed eyes and had never seen the world in depth, Li says: “Once she found out she was able to see some 3D, she immediately began to cry.”
Hensch suggests that playing video games releases some of the brain's functional brakes. He notes that heightened attention, which often goes along with video-game playing, has been shown to increase the activity of acetylcholine — a surge that would counteract the damping effect of Lynx1.
Windows of opportunity
Researchers have begun experimenting with drugs to reopen the critical period. Hensch and David Hunter, an ophthalmologist at Boston Children's Hospital, received approval in May to begin a phase I clinical trial for treating amblyopia with a drug that increases the amount of acetylcholine in the brain.
A similar study9, published in 2010 and led by neuroscientist Michael Silver of the University of California, Berkeley, found that when people with normal vision are given a drug that increases acetylcholine levels, they show greater improvements in visual acuity than people given a placebo. And a group led by Lamberto Maffei, a neurobiologist at the Scuola Normale Superiore in Pisa, Italy, has begun phase II clinical trials for amblyopia with selective serotonin re-uptake inhibitors, a class of drugs often used to treat depression.
Such research makes it easy to imagine pills or shots that could aid recovery from a severe brain injury, for example, or make it easier to learn a new language or forget a terrifying memory. Lifting plasticity brakes might even be useful in treating complex disorders such as autism, says Hensch. He points to the difficulty children with autism have integrating input from multiple senses at once — when looking at a person's facial expressions while listening to them speak, for example. Such integration may require the critical periods for each sense to have occurred in a specific developmental sequence. “I think that autism is a good example of what can go wrong when these different sensory critical periods are mistimed,” he says — a view for which there is some experimental evidence10.
For now, however, when it comes to the neural basis of complex psychiatric conditions such as autism, the experimental evidence is limited. But if tests could be created to identify risk factors for some developmental disorders, says Hensch, physicians may one day be able to deploy biologically informed interventions during the critical period, taking advantage of the brain's plasticity to set development on the right course.
But no one in the field is suggesting that the brain's critical periods should be tampered with casually. “When you reopen a critical period, there is, of course, always the possibility of a worse outcome,” says Alvaro Pascual-Leone, a neurologist at Harvard Medical School, pointing out that disorders such as amblyopia occur because of harmful input during the original critical period.
And structural brakes are considerably more difficult to release than functional ones. In 2009, for example, researchers showed that chemically destroying PNNs in mice makes it easier to erase their fear memories, suggesting a potential treatment for conditions such as post-traumatic stress disorder11. But to do this in humans could cause widespread brain damage that would outweigh any benefits. After all, says Hensch, the mechanisms that the brain uses to shut down critical periods are very complex, and they require a substantial amount of energy, “which gives us a good sense that they've evolved for a reason”.
Stryker sounds a further note of caution. “I think it's a romantic notion that you can replicate the critical period later in life,” he says. “Some things just don't unhappen.” Nature




 del.icio.us
del.icio.us Digg
Digg

Post your comment